Researchers Find Novel Insight into Early Neuronal Deficits Leading to Angelman Syndrome
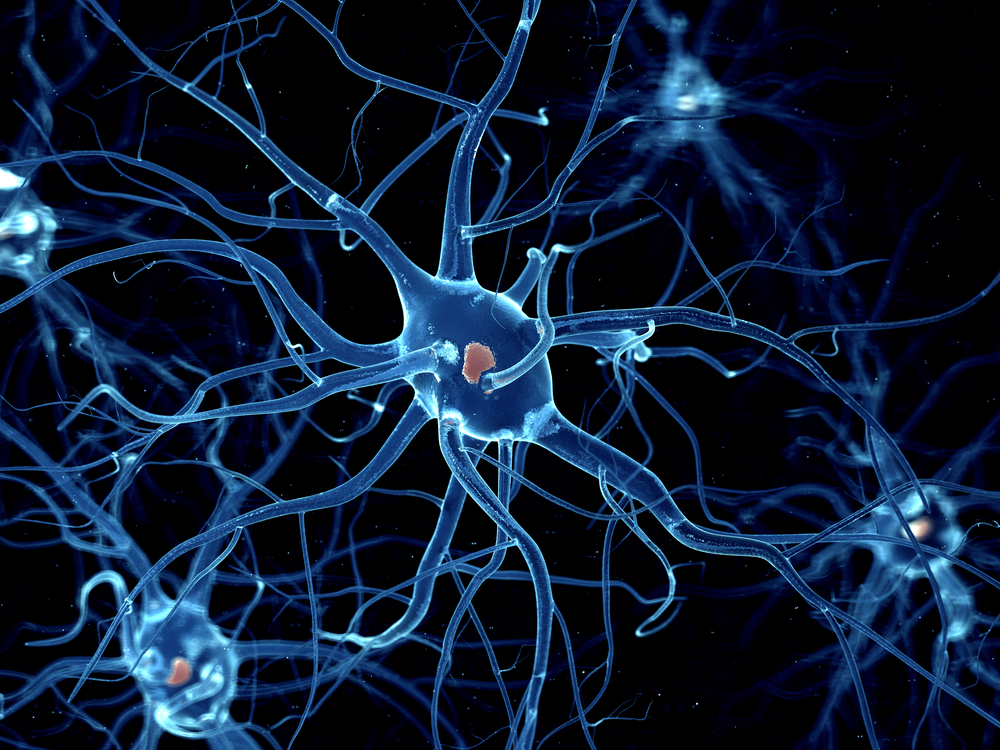
Researchers from the University of Connecticut School of Medicine have turned stem cells from patients with Angelman syndrome into neurons to investigate how the disease affects these cells.
The neurons had faulty maturation and electrical activity, as well as decreased ability to communicate with each other. In certain disease, low synaptic activity leads to profound brain deficits.
The study, “Disrupted neuronal maturation in Angelman syndrome-derived induced pluripotent stem cells,” appeared in the journal Nature Communications. It supports the use of stem cell-derived neurons as a valuable tool to uncover the mechanisms behind Angelman syndrome and test the potential treatments.
“We looked at the electrical activity of these brain cells and their ability to form connections, which is critical to the working circuits in the brain,” Eric Levine, the study’s principal researcher, said in a news release.
Angelman syndrome is caused by a missing maternal copy of the UBE3A gene. Researchers mimicked this in stem cell-derived neurons by deleting or blocking expression of this gene. The absence of this gene, they found, led to significant differences when compared to healthy stem cell-derived neurons.
“We found that the cells from Angelman patients had impairments,” Levine added. “They didn’t develop the same way as they do in people who don’t have the disorder. They failed to develop mature electrical activity and they didn’t form connections as readily.”
Importantly, these anomalies were rescued by promoting the expression of the paternal copy of the UBE3A gene.
“What’s interesting about this particular study is that Eric captured some of the first electrophysiological differences between Angelman syndrome neurons and typically developing neurons, and it appears those primary deficits are setting up all of the other problems that are happening [later in the disease],” said Stormy Chamberlain, a geneticist who contributed to the study.
According to Chamberlain, these changes are likely to occur during fetal development, so knowing exactly what happens is crucial in predicting what deficits patients will face during their lives.
The team also deleted the UBE3A gene from the DNA of cells from healthy donors to confirm its role in neuronal development.
“In the control subjects who did not have Angelman, we basically [deleted] the gene in order to mimic the Angelman defect,” said Levine. “If you do that early enough in development, you see all of the things go wrong in those cells. Interestingly, if you wait and [delete] the gene later in development, you only see a subset of those deficits.”
These results support the idea that UBE3A plays a crucial role in neuronal maturation, and also that the loss of proper neuronal communication is at the core of Angelman syndrome development. Levine believes that stopping initial electrical failure early may make it possible to halt progression of the disease.