After hesitation, we finally took steps to address our son’s disrupted sleep
'It’s just Angelman' no longer felt like a sufficient reason not to seek help
Written by |

When we received our son Jude’s Angelman syndrome diagnosis in April 2024, at just 16 months old, his geneticist warned us that disrupted sleep was to be expected. For many families, sleep disruption is a daily reality of the syndrome. It’s not only exhausting, but also brings the added anxiety of increased seizure risk. Poor sleep often leaves us on high alert the next day.
In the months following Jude’s diagnosis, we adapted to nights fractured by wakefulness. Between his first and second birthdays, Jude routinely woke between midnight and 3 a.m., kicking the sides of his cot or crawling energetically for hours. He didn’t require our help to resettle, but the noise alone made it nearly impossible for us to fall back asleep. Over time, the cumulative effects of sleep deprivation became apparent. I found it increasingly difficult to function safely and sustainably — driving to therapy appointments with a migraine, nodding off during my commute, and struggling to concentrate on daily tasks.
During a follow-up appointment at the Angelman clinic last September, shortly after Jude began seizure medication, we were asked if we had any other concerns. We hesitated. Jude’s sleep wasn’t ideal, but it didn’t feel “bad enough” to mention. We had come to accept disrupted sleep as an inevitable part of Angelman syndrome. But in reality, the broken nights were taking a significant toll, and “it’s just Angelman” no longer felt like a sufficient reason not to seek help.
Part of that shift came from realizing we were already working diligently to manage other seizure triggers, such as staying on top of gastrointestinal issues, doing our best to avoid illness and fevers, and making careful decisions about exposure when others were unwell. Addressing sleep felt like another essential piece of that puzzle.
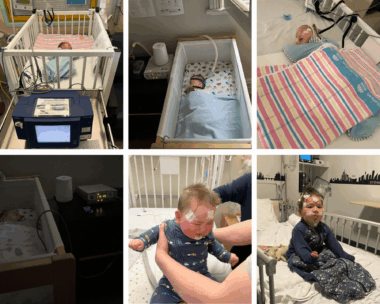
First row, from left: Jude has his first sleep study in the hospital at 3 weeks old; Jude sleeps with a CPAP mask, a rare occasion; Jude has a second sleep study at 2 months old. Second row, from left: Jude sleeps with an apnea monitor as a baby; Jude has his first overnight sleep study at 8 months old; Jude has his second overnight sleep study at 2 years old. (Photos by Joelene Wand)
I also took time to understand why sleep difficulties are so prevalent in Angelman syndrome. Learning that Jude’s disrupted sleep was rooted in neurological and biological factors — such as circadian dysregulation and melatonin secretion — rather than behavioral or parenting-related issues, eased some of my hesitation and self-doubt about seeking support.
Finally, I realized that Jude’s sleep challenges didn’t begin with his diagnosis. As a newborn, he was hospitalized for unexplained tachypnea and obstructive sleep apnea. He trialed a CPAP mask as an infant, slept with an apnea monitor as a baby, and underwent six overnight sleep studies — four in the hospital and two oximetry studies at home. His sleep had long been under medical scrutiny, so seeking specialist input was not a failure or a last resort, but rather a continuation of his care.
Since September, we’ve investigated Jude’s tonsils and adenoids, treated his iron deficiency, and started him on sleep medication. It hasn’t been a cure, and we still have occasional nights when Jude struggles to stay asleep. Like starting seizure medication, choosing to medicate for sleep wasn’t an easy decision. Yet over the past few months, I’ve noticed Jude is more alert and engaged during the day, a change his therapists have also observed.
For our family, the impact of poor sleep on Jude’s health — and on our own safety and well-being — was becoming unsustainable. Asking for help with sleep felt daunting, especially in a community where so many caregivers are already stretched beyond capacity. But for both Jude and us, taking steps to address his disrupted sleep was one of the most compassionate choices we could make.
Note: Angelman Syndrome News is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website. The opinions expressed in this column are not those of Angelman Syndrome News or its parent company, Bionews, and are intended to spark discussion about issues pertaining to Angelman syndrome.




iana jacobson
We've struggled with sleep issues with our 14 year angelman girl since she was 2 years old. She takes melatonin and epilepsy meds . She falls asleep at around 10pm but always wakes up every night between 2am and 4am. Making her bedtime later makes no difference. She spends her waking time watching tv (It's the only thing that will keep her from shouting at the top of her voice) She may or may not go back to sleep. She is happy to fall back asleep (should she wish) with the tv on.
She has had 3 sleep studies and has been the worst sleeper on all of them.
We've given up trying to find a solution.
Donna Clavette
OMG, my daughter is 37 and I still remember how much we went through ..sleep was a major issue. Wonder how we ever survived finally at the age of 21 she was put on trazodone just a small amount prior to that. It was like clockwork 2 o’clock in the morning four hours of sleep at least five days a week I wonder how I did it and survived. I can’t tell you how wonderful it is to have my sleep back.!! We are all strong parents!!
Sabrina Johnson
Hi Iana--I love the part about shouting at the top of her voice :) I thought we were the only family experiencing this. Our daughter is 15 and is often up at 5 am. Which is great compared to 3 am. We have a camera in her room, and when I can see that all is well, I go back to sleep. She eventually plays with her toys or listens to music. It's still a challenge when she wakes up and everyone else planned to sleep in. Naps have been a saving grace for me to get a little restoration when she's had a busy night.