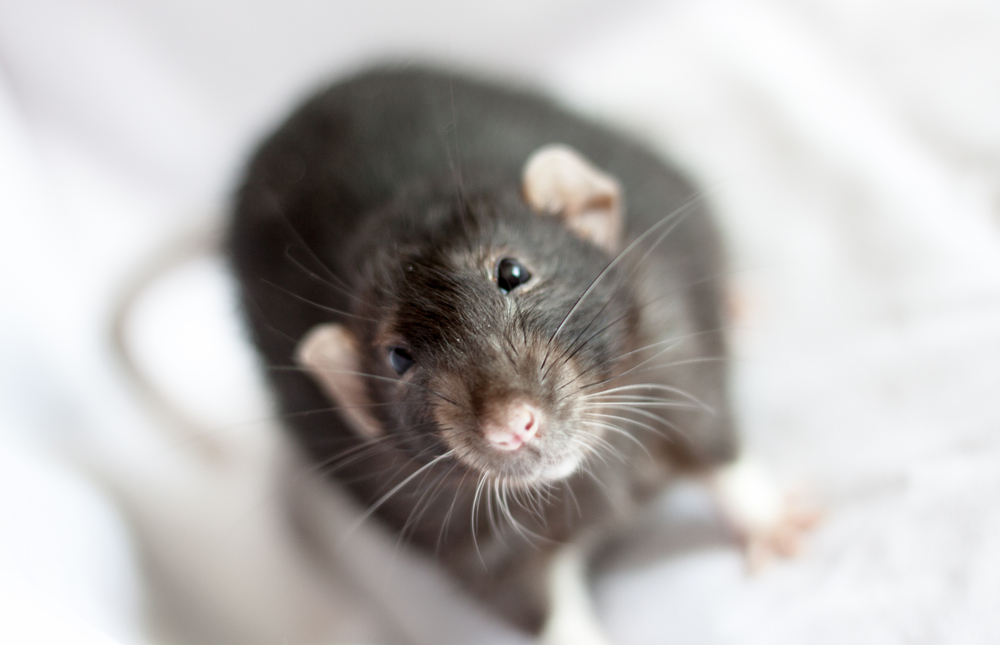
Reactivating UBE3A May Reverse Changes in Brain in Angelman Syndrome, Study In Mice Shows
Written by |
Angelman syndrome is caused by a lack of functional UBE3A gene in the brain. Thus, getting brain cells to express a functional UBE3A gene seems like a fairly intuitive therapeutic strategy. Yet at what point during disease progression must UBE3A be introduced in order to avoid the changes seen in Angelman syndrome?
A new study using a mouse model of Angelman syndrome reports that restoring the UBE3A gene in the brains of adult mice is sufficient to reverse some of the changes in brain physiology that accompany this disease, suggesting that expressing this gene in the brain may be beneficial even if the brain is already fully developed.
The study, “Adult Ube3a Gene Reinstatement Restores the Electrophysiological Deficits of Prefrontal Cortex Layer 5 Neurons in a Mouse Model of Angelman Syndrome,” was published in The Journal of Neuroscience.
The researchers behind the new study had previously developed a mouse model of Angelman syndrome where the UBE3A gene is “turned off;” however, it could be turned “back on” at any point during development. Using this model, they demonstrated that reactivating UBE3A as late in development as adolescence could reduce motor problems. However, anxious behaviors and epilepsy were only prevented if UBE3A was reactivated early in development.
“It is possible that the hitherto largely unsuccessful therapeutic clinical trials for neurodevelopmental disorders are to some extent caused by administering interventions outside the boundaries of the therapeutic window,” the investigators said.
In this study, the team examined how the brains of their model mice differed from those of wild-type mice. In some parts of the mouse brain, a lack of UBE3A caused there to be more signals that activate neurons and fewer signals that inhibit them.
Some types of neurons in UBE3A-lacking mouse brains were less excitable (less likely to be activated to send signals of their own).
Excitatory and inhibitory neural signals are the “yin and yang” of the brain. Excitatory signaling from one nerve cell to the next makes the latter cell more likely to fire an electrical signal. Inhibitory signaling makes the latter cell less likely to fire. This is the basis of communication between nerve cells in the brain.
Interestingly, when the researchers reactivated UBE3A in the brains of adult mice, these physiological changes in neurons associated with UBE3A loss were gradually reversed, and completed at six weeks after gene reactivation.
This finding is somewhat paradoxical, as the investigators had previously shown that reactivating UBE3A did not reverse behavioral changes.
The researchers think this probably has to do with other changes happening in UBE3A-deficient brains that they didn’t identify in this study, which focused primarily on the region of the brain known as the prefrontal cortex — a region involved in the regulation of thoughts and actions in accordance with internal goals, such as decision making or social behavior.
Changes in other regions of the brain — and even changes in this region that the researchers didn’t or couldn’t study — are the most likely reasons for this mismatch between the improved brain physiology and the persistent symptoms.
Still, this study does show that gene-based therapies of this kind can, at least in lab models, have measurable effects even after the brain is fully developed.