Chaotic Brain Activity Pattern May Be Early Marker of Angelman Syndrome, Case Study Reports
Written by |
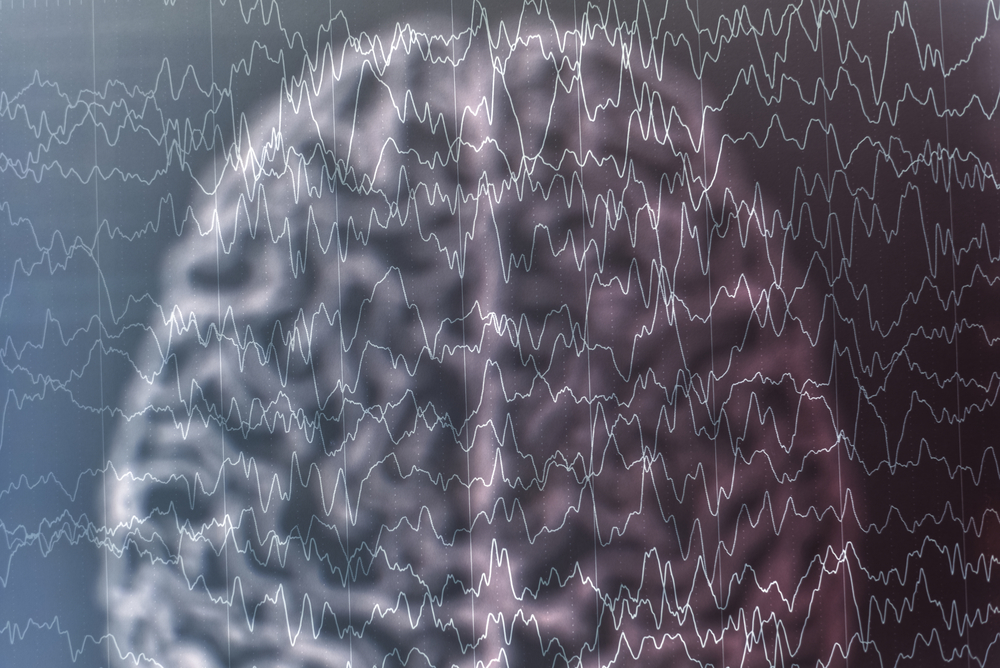
Hypsarrhythmia — disorganized and chaotic brain activity with no recognizable pattern — may be an early marker of Angelman syndrome, according to a case study.
The report, “Pseudo Hypsarrhythmia: An Early Marker of Angelman Syndrome,” was published in the Annals of Indian Academy of Neurology.
Although seizures may appear in patients as early as one month old, symptoms of Angelman syndrome only become fully evident after age 3 or 4, making it hard to diagnose this disorder early on.
Hypsarrhythmia is chaotic and disorganized brain electrical activity that has no recognizable pattern. This contrasts with normal brain electrical activity, which presents a separation between each brain wave signal and originates a clear pattern visible on an electroencephalogram (EEG). Hypsarrhythmia is the most common EEG pattern associated with infantile spasms.
The first case of hypsarrhythmia in a patient with Angelman was reported in 1973; similar reports have been extremely rare worldwide. As such, the link between hypsarrhythmia and Angelman remains poorly recognized.
In the study, researchers from India described an 18-month-old child who experienced language delay and recurrent seizures at 12 months.
Her mother’s pregnancy was uneventful. The patient’s development was normal except for her language skills. While able to listen and recognize common words, she was only able to express herself verbally with gurgling sounds and babbling.
She also experienced increasingly frequent generalized tonic seizures — characterized by stiff muscles and jerky movements — and teeth grinding. Her parents had also noticed the appearance of generalized trembling and failure to achieve new milestones.
At 18 months, she was able to take a few steps if holding on to furniture, pick up small objects, and wave goodbye. Yet, her speech was unclear, she used gestures to communicate, and she still babbled.
At examination, she was easily excitable and had frequent unprovoked episodes of laughter. Her mouth was always open with a protruded (stuck out) tongue. The patient also had involuntary jerky movements of her arms and legs. Her head circumference suggested microcephaly, meaning a head that was smaller than normal.
On neurological examination, she revealed mild generalized hypotonia, or low muscle tone, although a magnetic resonance imaging of the brain showed normal results.
In line with her first exam at 12 months, a repeat EEG — a method to record electrical brain activity — showed changes that suggested hypsarrhythmia.
A genetic technique known as fluorescence in situ hybridization found a deletion on chromosome 15 (15q11–q13), which confirmed a diagnosis of Angelman syndrome. The patient subsequently started on a neurorehabilitation program, using anti-epileptic treatment to control her seizures.
Overall, these results suggest that hypsarrhythmia may be “a clue to the early diagnosis of [Angelman syndrome] in infants and toddlers,” the researchers wrote.
“Early detection in very young children … provides the opportunity for early intervention, genetic diagnosis, and prenatal counseling,” they said.