Cells Used to Model Angelman Syndrome in Labs May Have Genetic Defect, Study Contends
Written by |
Sergey Nivens/Shutterstock
Researchers have found a specific type of genetic defect in stem cells derived from a patient with Angelman syndrome that have been used as a laboratory model to study the disease.
The team claims that such alterations might have serious implications and should be taken into account when selecting this type of approach for disease modeling.
The study, “Loss of hierarchical imprinting regulation at the Prader-Willi/Angelman syndrome locus in human iPSCs,” was published in Human Molecular Genetics.
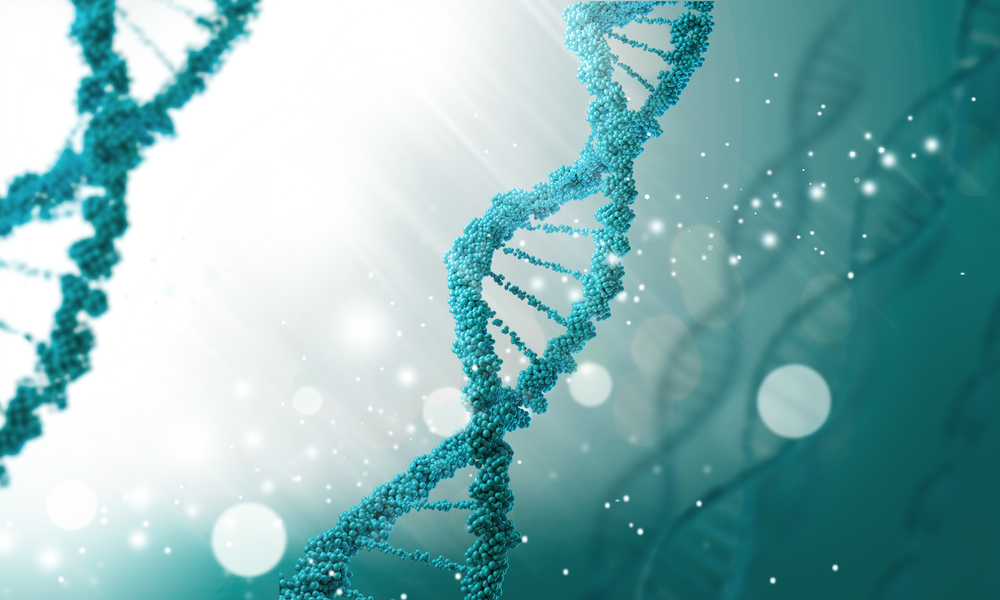
Genomic imprinting is the process by which one copy of a gene, either the maternal or paternal copy, is silenced by a chemical DNA modification called methylation.
In mammals, these imprinted genes typically cluster in specific regions of chromosomes, such as the human chromosome 15 (chr15q11-q13), that contains a set of imprinted genes associated with two
neurodevelopmental disorders: Angelman syndrome (AS, caused by a loss of function of maternal genes); and Prader-Willi syndrome (PWS, caused by a loss of function of paternal genes).
Regulation of imprinted genes usually is mediated by imprinting centers (ICs), which are special DNA regulatory regions located next to the genes under their control. In the case of the human chr15q11-q13 there are two different ICs: the AS-IC, that activates maternal imprinted genes; and the PWS-IC, that activates paternal imprinted genes.
In recent years, scientists have been trying to develop an in vitro model system to study these imprinted disorders in the laboratory. Induced pluripotent stem cells (iPSCs) are extremely useful to use as a disease model in a culture dish. iPSCs are reprogrammed patient-derived cells that can give rise to almost any cell type in the body.
Cell reprogramming can be compared to erasing and reformatting a computer hard-drive. It erases the genetic “memory” of that cell, making it go back to a naive state. It then has the potential to become a completely different cell type.
However, in the case of imprinted diseases, the use of iPSCs to model these disorders might not be straightforward, since many iPSCs carry several imprinting defects that could potentially introduce confusion and bias in the system.
In this study, investigators reprogrammed skin cells from an Angelman patient and an age-matched healthy control subject and generated several iPSCs lines to evaluate their imprinting stability across the PWS/AS domain.
To this end, they focused on three different DNA regulatory regions that are normally methylated (silenced) on the maternal allele: the PWS imprinting center (PWS-IC), and the NDN and MKRN3 genes that are under the control of the PWS-IC.
While PWS-IC retained its normal methylation pattern in most iPSCs lines tested, one of five control iPSC lines showed loss of maternal methylation in multiple imprinted genes from the PWS/AS domain.
Unlike NDN, MKRN3 was abnormally hypermethylated (over-silenced) in all control and Angelman iPSCs lines, regardless of the PWS-IC methylation status, suggesting that these iPSCs lose the hierarchical control of imprinted genes at the PWS/AS domain.
“These results highlight, for the first time, a change in the hierarchy of imprinting regulation within imprinted domains in iPSCs,” the authors wrote.
The findings were confirmed using different reprograming techniques to generate iPSCs.
Altogether, these findings indicate that hierarchical imprinting does not occur in iPSCs, which may explain to some degree the prevalence of imprinting defects in these reprogrammed stem cells. Authors also highlighted such alterations should be taken into account when using iPSCs in disease modeling.